Thursday, December 8, 2011
Thursday, October 6, 2011
Just Remember I Love You
Over the weekend I completed the LiveStrong ride and event here in South Florida. Although having a few bumps being the inaugural event, it came off splendidly. I ended up riding the short course with my wife and her good friend. I was originally afraid to ride because these things are usually crash fests, but with most riders doing the 100k or 30 mile ride there was only a small group to do the symbolic 10.2 mile ride. It actually made a funny picture with half a dozen police cruisers surrounding just the three of a us, blocking traffic on A1A in north Miami beach, after the group spread out and everyone else but us left the police escort behind. I've never felt more safe on two wheels. I can't imagine what $215,000 will buy for LiveStrong. How many guidebooks or staff hours spent directing those diagnosed with cancer into clinical trials or helping navigate insurance options. It's an amazing thing.
Some good news, the medical team has OK'd me to return to work on Monday. I had my six weeks scans in Houston yesterday, and the results were neither here nor there - as expected at this juncture. They could have been worse, they certainly could have been better. In fact, they were good enough to keep me in the TIL clinical trial but also bad enough to consider leaving the trial and starting option B (or D, or E - I've lost track). Ah, the ambiguity of cancer treatment. I have further scans in another six weeks that will be important in determining whether the TIL treatment was successful or not, should I decide to wait. In the meantime life seems to slowly be returning to some level of normalcy, although I'm not sure what I expect normal to be these days. I think about this a lot. I am not equal, physically, to what I was before the fight began. There are aches and pains, some body parts don't function as well as they did and stamina is fleeting. But does this mean I am worse off than when I began? Or is it something to be treated or accepted in kind? Should I complain or rejoice? I have resorted to asking myself "what would John Wayne do?" I use this as a litmus test as to the degree of 'nutting up' that is required for any given situation. Would John Wayne complain about aches and pains? I think not. Perhaps this is the new normal, or perhaps it will get better. Either way, it is what it is.
I have to admit that I am a little afraid to return to something like a normal life. Any survivor - and anyone living with cancer is a survivor - has to question why it is that they survived. What did they survive for? I am sure that there'll come a point, perhaps at a dismal business meeting in some god forsaken town, where I will ask myself "I survived for this?" I have given a lot of thought to this and I believe the answer will definitely be 'yes'. We survive for everything that is life, the small things, the big things, the good and the bad. Because the dead only know one thing, that it is better to be alive. It is better to know anything then it is know nothing. And to be honest, I quite fancied my life before my battle with cancer began - the good, bad, big and small. I will gladly take the little things, the bad things, again if I could only just maintain my role as my children's father. That alone is worth everything, and my family is the reason I fought so hard this summer. Fittingly, our family anthem is the 70s song "Just Remember I Love You". For some reason, my kids absolutely love that song and the lyrics have been keenly appropriate this year. There is nothing sweeter in the world than my six-year-old singing to me "just remember I love you, and it'll be all right". I remember, believe me I remembered during the endless hours in the hospital bed staring at the picture of her precious face knowing that I had to pull through for her.
So - since I do not have much going on for at least the next month on the cancer front - this will be my last post for a while, perhaps longer. I'm getting back to a normal life and hopefully for good. If you haven't already, sign up for e-mail notification of any future blog updates. I cannot even begin to thank all my readers for your support. Many I know, most I do not. However, each and every one has meant very much to me and all have had a hand in this great fight. Unfortunately, the fight continues. Not just for me but also for the 28 million other people affected by cancer in the world today. October is breast cancer awareness month and, sadly, my mother was diagnosed with breast cancer just a short time ago. She begins chemotherapy treatment next week in her hometown. As if I do not have enough reasons to hate cancer - now one half of my birth family is going through cancer treatment. Her prognosis is good though, and she is a tough old bird - but it still pisses me off. There are way to many affected by cancer in the world today, it's just unacceptable.
Let's agree that in the meantime you will continue to do your part, fighting for yourself or a loved one or just out of kindness for others. I'll continue my fight, kicking cancer's ass in my own backyard. Until next time.
"When it all goes crazy and the thrill is gone,
The days get rainy and the nights get long,
And you get that feeling you were born to lose
Staring at your ceiling thinking of your blues.
When there's so much trouble that you want to cry
The world has crumbled and you don't know why
When your hopes are fading and they can't be found
Dreams have left you waiting, friends have let you down.
Just remember I love you, and it will be all right.
Just remember I love you more than I can say.
Maybe then your blues will fade away."
"When the blues come calling at the break of dawn
The rain keeps falling but the rainbow's gone
When you feel like crying but the tears won't come
When your dreams are dying, when you're on the run.
Just remember I love you and it will be all right."
I do, and it certainly is.
Some good news, the medical team has OK'd me to return to work on Monday. I had my six weeks scans in Houston yesterday, and the results were neither here nor there - as expected at this juncture. They could have been worse, they certainly could have been better. In fact, they were good enough to keep me in the TIL clinical trial but also bad enough to consider leaving the trial and starting option B (or D, or E - I've lost track). Ah, the ambiguity of cancer treatment. I have further scans in another six weeks that will be important in determining whether the TIL treatment was successful or not, should I decide to wait. In the meantime life seems to slowly be returning to some level of normalcy, although I'm not sure what I expect normal to be these days. I think about this a lot. I am not equal, physically, to what I was before the fight began. There are aches and pains, some body parts don't function as well as they did and stamina is fleeting. But does this mean I am worse off than when I began? Or is it something to be treated or accepted in kind? Should I complain or rejoice? I have resorted to asking myself "what would John Wayne do?" I use this as a litmus test as to the degree of 'nutting up' that is required for any given situation. Would John Wayne complain about aches and pains? I think not. Perhaps this is the new normal, or perhaps it will get better. Either way, it is what it is.
I have to admit that I am a little afraid to return to something like a normal life. Any survivor - and anyone living with cancer is a survivor - has to question why it is that they survived. What did they survive for? I am sure that there'll come a point, perhaps at a dismal business meeting in some god forsaken town, where I will ask myself "I survived for this?" I have given a lot of thought to this and I believe the answer will definitely be 'yes'. We survive for everything that is life, the small things, the big things, the good and the bad. Because the dead only know one thing, that it is better to be alive. It is better to know anything then it is know nothing. And to be honest, I quite fancied my life before my battle with cancer began - the good, bad, big and small. I will gladly take the little things, the bad things, again if I could only just maintain my role as my children's father. That alone is worth everything, and my family is the reason I fought so hard this summer. Fittingly, our family anthem is the 70s song "Just Remember I Love You". For some reason, my kids absolutely love that song and the lyrics have been keenly appropriate this year. There is nothing sweeter in the world than my six-year-old singing to me "just remember I love you, and it'll be all right". I remember, believe me I remembered during the endless hours in the hospital bed staring at the picture of her precious face knowing that I had to pull through for her.
So - since I do not have much going on for at least the next month on the cancer front - this will be my last post for a while, perhaps longer. I'm getting back to a normal life and hopefully for good. If you haven't already, sign up for e-mail notification of any future blog updates. I cannot even begin to thank all my readers for your support. Many I know, most I do not. However, each and every one has meant very much to me and all have had a hand in this great fight. Unfortunately, the fight continues. Not just for me but also for the 28 million other people affected by cancer in the world today. October is breast cancer awareness month and, sadly, my mother was diagnosed with breast cancer just a short time ago. She begins chemotherapy treatment next week in her hometown. As if I do not have enough reasons to hate cancer - now one half of my birth family is going through cancer treatment. Her prognosis is good though, and she is a tough old bird - but it still pisses me off. There are way to many affected by cancer in the world today, it's just unacceptable.
Let's agree that in the meantime you will continue to do your part, fighting for yourself or a loved one or just out of kindness for others. I'll continue my fight, kicking cancer's ass in my own backyard. Until next time.
"When it all goes crazy and the thrill is gone,
The days get rainy and the nights get long,
And you get that feeling you were born to lose
Staring at your ceiling thinking of your blues.
When there's so much trouble that you want to cry
The world has crumbled and you don't know why
When your hopes are fading and they can't be found
Dreams have left you waiting, friends have let you down.
Just remember I love you, and it will be all right.
Just remember I love you more than I can say.
Maybe then your blues will fade away."
"When the blues come calling at the break of dawn
The rain keeps falling but the rainbow's gone
When you feel like crying but the tears won't come
When your dreams are dying, when you're on the run.
Just remember I love you and it will be all right."
I do, and it certainly is.
Friday, September 23, 2011
Undead
Something else I did this week was to watch Charlie Sheen's roast on television. I believe that life’s lessons can be found as easily in the gutter as on the windswept mountaintops or the self-help section of a bookstore. Those who do not believe this miss out on quite a few opportunities to learn a few things. So whatever you may think of Charlie and his recent troubles, I think his summer holds a lesson for us all. Successful people – and we cannot deny his success just because we disagree with how he celebrated that success – tend to do successful things. At the apparent end of his crazy train ride he moved forward, not backwards. He laughed at himself, learned from the experience and moved on. He did not execute a reversal or a return to some previous self, but moved forward. This seems to be evident in a newfound appreciation for what is good in his life, a renewed love for those who love him. He appears to be turning a potentially lethal episode into a chance to improve himself. In his own words, "I'm done with 'winning' because I've already won."
This phrase stuck in my mind this week because I’ve recently claimed in this space to be “winning” but am realizing that I, too, have already won. Both in terms of learning valuable life lessons from a traumatic episode and also from passing a milestone in my battle with cancer. A year ago today I made an appointment with my optometrist because I was having unexplained limited field of vision in my right eye. This would eventually be exposed as a tumor and my initial cancer symptom. Stage 4 melanoma cancer patients live, on average, one year past their initial symptoms of the disease. There is nothing absolute about that number or date, or any such statistic, but that's how my situation was framed by the oncologists when I was diagnosed. That wound up the countdown clock that started ticking in the back of my mind. For what it is worth, today I am now past that dreaded milestone. I have now beaten those particular odds. And cancer has already left me a much better person - a little worse for wear, but a better human being then when I started. I have a newfound appreciation for my life, for my loved ones and for the great adventure upon which I continue. And I’m not only still here, I'm very much not dead. At the Melanoma Research Foundation's online community the stage 4’s that have beaten the odds are called the “undead.” So that’s me, from today onward - the undead. May I wish myself many happy returns.
Still, we always need to keep our eyes on the prize as we pass such milestones. For me that prize is having the three best letters is the alphabet – NED – entered in my medical records. NED, or ‘no evidence of disease’, is the closest you can get to being declared cured of cancer. That goal feels more real than ever now, and I swear I can almost see it if I look hard enough. I move towards it now with increased determination, with a little more energy in my steps, because I've already beaten the initial odds against me. What else can I do?
So time for a score update: William 1, cancer 0.
Sunday, September 18, 2011
Details, Details
I have had a lot of questions on the details of my treatment, what is it like to go through (aggressive) cancer treatment? I have avoided it until now, but here goes. My conclusions are in the last two paragraphs if details are not your thing, I won't be offended if you skip ahead. The biochemotherapy was very complex so that would be too difficult to explain, so I'll take you through a course of high-dose IL2 I received after my t-cell replacement. Join me on a not so pleasant cancer treatment journey, a week in the life if you will.
Jerry Seinfeld had a joke about how there is no normal strength pain medication any more? There is "extra strength" and "super strength" but nothing normal. His suggested solution to figuring out what strength he needed was to ask his doctor to figure out what would kill him and then "back off just a little bit." That is kind of like IL2 treatment for melanoma, because you can get up to 12 doses of the stuff but most people get 3-7 as best as I can assess. The question of how much they give you is much like Seinfeld's joke, and is surprisingly as much art as it is science.
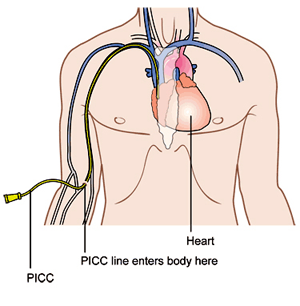
So you start by checking into the hospital, which can be an adventure all on its own. At MD Anderson they like to start IL2 patients on Mondays and give the doses every eight hours; at 9am, 5pm and 1am. You always have this in the back of your head when checking in but you are most likely going to start at 9am the next day - but maybe earlier. It makes it hard to brace yourself for what is coming when you don't know when it is coming. And there is the administrative nonsense, the paperwork, the overwhelming feeling of being a cancer patient when you walk into the massive building full of bald people toting around IV poles. You get into your room, unpack and make ready for whatever they throw at you. But first you must get connected to the machines so that you can become a bald person toting around an IV pole. There is the IV link to your PICC line (see diagram) that delivers the drugs directly to your heart. You usually keep the PICC line in between treatments, it's your semi-permanent plug-n-play that's stays with you most of the time you are in treatment. There is the cardio measurement which is five wires connected to tabs stuck on your chest. Then there is the oxygen monitor that is affixed to your finger. And then the blood pressure cuff on your arm. That is eight wires dangling off your body as you sleep, go to the bathroom, walk around the room, twenty four hours a day.
Your first dose at 9am so you start to brace yourself. By then you've met your nurse and assistant nurse, the floor nurse has probably stopped by and the doctors have made their daily rounds with you. They size you up to see what kind of week they will be having with you. You put up a strong face and try to act appreciative, like being friendly to the pilot on the airplane for no reason except that it seems like something that may help your situation. Then you wait, maybe an hour or five minutes or an hour and a half, until two nurses in biological warfare suits walk in with bags and bags of toxic, lifesaving drugs. For IL2 it takes 15 minutes for the drugs to flow into your system through your IV line. Then you watch the TV with one eye on the clock, the nurses and your caregiver in your room at the ready. They smile at you but you know they are also bracing for the storm of side effects that, in many ways, hurts them as much as you - especially if the caregiver is a parent or other loved one. My Gatorade made cold, hot blankets at quick access and the nurses armed with pre-approved multiples doses of demerol and dilaudid (both are opioids similar to morphine) - I'm ready as I can be. While my symptoms actually varied over my two courses of IL2, my first course had the same side effects after each dose. In these, at one hour, almost to the minute after the administration of the IL2, I would start to chill. Not Jimmy Buffet on a beach kind of chill, but as if someone tossed me naked into an ice bath. I'm talking the movie Titanic type cold that starts in your bones and works its way out. This takes hold in about half a minute and the hot blankets get piled on. The first injection of demerol helps give a feeling of warmth almost immediately but then the shakes start. The medical term is "hard rigors" and it is basically violent shaking from head to toe, in a kind of fetal position grabbing my knees and trying to control the outbursts from my own muscles. My bed shook so bad I swear it moved across the floor, my teeth chattered so hard I damaged my dental work and my heart beat so fast that I developed arrhythmias as I slept later that night. I could not talk during this, and I focused mainly on not hyperventilating which was about all I could do. This went on for one to two hours until the combination of successive and alternating opiate injections mollified my muscles enough to make them stop contracting and I fell off to half sleep. After each dose I felt like I had just completed a bike race, and with my heart rate averaging 165-190 bpm for an hour to two at a time that is the cardio equivalent of a fifty mile bike race for me - just a little harder effort.
So, in five hours you get to ask the question - do we do another dose or call it quits? The doctors assess the effects, they query you on how you feel, they see how much water your body has retained and how much fluid has gotten into your lungs (a side effect of IL2 is fluid leaking into other parts of your body). After my fourth treatment I was on oxygen full time. Part of my lung's lower lobes actually had collapsed which further complicated my breathing. Breathing is good, not breathing is not so good. The cardiologist had visited a few times and was on call for me. He put paddles permanently on my chest in case he needed to shock my heart during treatments. Really? It's late at night and the doctor called from home, the nurse said that he wanted to talk to me on the phone. He explained that this was a clinical trial - there are no "normal" results and that he could not say if my next dose would be easier or harder. He wanted to know if I could take another treatment, that he was going to green-light it medically but needed me to be on board. Gut-check time, DuPree. I said yes, one more. When the nurses brought in those toxic bags I started to regret my decision, honestly I did. But it was time to nut up or shut up, so I did it and then passed out to oblivion.
That was my fifth and last dose that course, but it is not over yet. The side effects of the treatment need to be addressed before you go home. That may take a day, or three or a week. You gain up to 20% of your body weight in extra fluids, your organs start to hiccup and they need to be coaxed back to normal function. Your skin may blotch and peel uncontrollably, turning an itchy fire red. Your digestive system protests and you get to discuss your bowel movements and urine output in great detail to any medical staff who comes in your room. And its 24 hours a day, every day, without break. Temperature and weight at 3am, blood draw at 4am, drugs at 5am, new nurse at 7am, around the clock. You can walk the floor to get out of the confines of your room but that does not free you too much. It is 302 steps to circumnavigate my floor of 32 rooms, plus or minus 6 steps. And so it goes, day after boring day, waiting for the magical word "discharge" to free you. Until you come back again for another treatment and start it all again. Next time may be easier, or it may be more difficult in a myriad of ways. Each treatment is different for each person, but it is rarely easy.
So this is what I mean when I say I'm fighting cancer. Cancer warriors do not check into a cancer treatment unit, hook up to an IV, sit back and hope for the best. No. They choose the aggressive treatment option over the standard treatment, they choose the clinical trial if they have to. They say "yes" when the doctors ask if they can take any more pain. They take control of their non-treatment time with exercise and diets. They research treatment options and choose their medical teams. They choose to sit up in their hospital beds instead of laying down, to walk with the IV pole instead of staying in bed whenever they can. They put on brave faces when sharing their cancer stories. They swallow the pain, the indignity, and the fear to be brave around another cancer warrior or care giver feeling down. They walk back into these hospital rooms over and over and over again. They start every day as I do, saying "I'm still alive - so fuck you cancer."
I guess I did not want to write this because I did not want cancer thinking we are having a tough time fighting. But you are right to ask me to share this. You have joined the fight against cancer if you are reading this, and I know that you can handle the truth. Just remember that in every fight - no matter how costly or how lengthy or how horrific - there is a victor. And cancer will not stand victorious after these battles. No way, no how.
Jerry Seinfeld had a joke about how there is no normal strength pain medication any more? There is "extra strength" and "super strength" but nothing normal. His suggested solution to figuring out what strength he needed was to ask his doctor to figure out what would kill him and then "back off just a little bit." That is kind of like IL2 treatment for melanoma, because you can get up to 12 doses of the stuff but most people get 3-7 as best as I can assess. The question of how much they give you is much like Seinfeld's joke, and is surprisingly as much art as it is science.
So you start by checking into the hospital, which can be an adventure all on its own. At MD Anderson they like to start IL2 patients on Mondays and give the doses every eight hours; at 9am, 5pm and 1am. You always have this in the back of your head when checking in but you are most likely going to start at 9am the next day - but maybe earlier. It makes it hard to brace yourself for what is coming when you don't know when it is coming. And there is the administrative nonsense, the paperwork, the overwhelming feeling of being a cancer patient when you walk into the massive building full of bald people toting around IV poles. You get into your room, unpack and make ready for whatever they throw at you. But first you must get connected to the machines so that you can become a bald person toting around an IV pole. There is the IV link to your PICC line (see diagram) that delivers the drugs directly to your heart. You usually keep the PICC line in between treatments, it's your semi-permanent plug-n-play that's stays with you most of the time you are in treatment. There is the cardio measurement which is five wires connected to tabs stuck on your chest. Then there is the oxygen monitor that is affixed to your finger. And then the blood pressure cuff on your arm. That is eight wires dangling off your body as you sleep, go to the bathroom, walk around the room, twenty four hours a day.
Your first dose at 9am so you start to brace yourself. By then you've met your nurse and assistant nurse, the floor nurse has probably stopped by and the doctors have made their daily rounds with you. They size you up to see what kind of week they will be having with you. You put up a strong face and try to act appreciative, like being friendly to the pilot on the airplane for no reason except that it seems like something that may help your situation. Then you wait, maybe an hour or five minutes or an hour and a half, until two nurses in biological warfare suits walk in with bags and bags of toxic, lifesaving drugs. For IL2 it takes 15 minutes for the drugs to flow into your system through your IV line. Then you watch the TV with one eye on the clock, the nurses and your caregiver in your room at the ready. They smile at you but you know they are also bracing for the storm of side effects that, in many ways, hurts them as much as you - especially if the caregiver is a parent or other loved one. My Gatorade made cold, hot blankets at quick access and the nurses armed with pre-approved multiples doses of demerol and dilaudid (both are opioids similar to morphine) - I'm ready as I can be. While my symptoms actually varied over my two courses of IL2, my first course had the same side effects after each dose. In these, at one hour, almost to the minute after the administration of the IL2, I would start to chill. Not Jimmy Buffet on a beach kind of chill, but as if someone tossed me naked into an ice bath. I'm talking the movie Titanic type cold that starts in your bones and works its way out. This takes hold in about half a minute and the hot blankets get piled on. The first injection of demerol helps give a feeling of warmth almost immediately but then the shakes start. The medical term is "hard rigors" and it is basically violent shaking from head to toe, in a kind of fetal position grabbing my knees and trying to control the outbursts from my own muscles. My bed shook so bad I swear it moved across the floor, my teeth chattered so hard I damaged my dental work and my heart beat so fast that I developed arrhythmias as I slept later that night. I could not talk during this, and I focused mainly on not hyperventilating which was about all I could do. This went on for one to two hours until the combination of successive and alternating opiate injections mollified my muscles enough to make them stop contracting and I fell off to half sleep. After each dose I felt like I had just completed a bike race, and with my heart rate averaging 165-190 bpm for an hour to two at a time that is the cardio equivalent of a fifty mile bike race for me - just a little harder effort.
So, in five hours you get to ask the question - do we do another dose or call it quits? The doctors assess the effects, they query you on how you feel, they see how much water your body has retained and how much fluid has gotten into your lungs (a side effect of IL2 is fluid leaking into other parts of your body). After my fourth treatment I was on oxygen full time. Part of my lung's lower lobes actually had collapsed which further complicated my breathing. Breathing is good, not breathing is not so good. The cardiologist had visited a few times and was on call for me. He put paddles permanently on my chest in case he needed to shock my heart during treatments. Really? It's late at night and the doctor called from home, the nurse said that he wanted to talk to me on the phone. He explained that this was a clinical trial - there are no "normal" results and that he could not say if my next dose would be easier or harder. He wanted to know if I could take another treatment, that he was going to green-light it medically but needed me to be on board. Gut-check time, DuPree. I said yes, one more. When the nurses brought in those toxic bags I started to regret my decision, honestly I did. But it was time to nut up or shut up, so I did it and then passed out to oblivion.
That was my fifth and last dose that course, but it is not over yet. The side effects of the treatment need to be addressed before you go home. That may take a day, or three or a week. You gain up to 20% of your body weight in extra fluids, your organs start to hiccup and they need to be coaxed back to normal function. Your skin may blotch and peel uncontrollably, turning an itchy fire red. Your digestive system protests and you get to discuss your bowel movements and urine output in great detail to any medical staff who comes in your room. And its 24 hours a day, every day, without break. Temperature and weight at 3am, blood draw at 4am, drugs at 5am, new nurse at 7am, around the clock. You can walk the floor to get out of the confines of your room but that does not free you too much. It is 302 steps to circumnavigate my floor of 32 rooms, plus or minus 6 steps. And so it goes, day after boring day, waiting for the magical word "discharge" to free you. Until you come back again for another treatment and start it all again. Next time may be easier, or it may be more difficult in a myriad of ways. Each treatment is different for each person, but it is rarely easy.
So this is what I mean when I say I'm fighting cancer. Cancer warriors do not check into a cancer treatment unit, hook up to an IV, sit back and hope for the best. No. They choose the aggressive treatment option over the standard treatment, they choose the clinical trial if they have to. They say "yes" when the doctors ask if they can take any more pain. They take control of their non-treatment time with exercise and diets. They research treatment options and choose their medical teams. They choose to sit up in their hospital beds instead of laying down, to walk with the IV pole instead of staying in bed whenever they can. They put on brave faces when sharing their cancer stories. They swallow the pain, the indignity, and the fear to be brave around another cancer warrior or care giver feeling down. They walk back into these hospital rooms over and over and over again. They start every day as I do, saying "I'm still alive - so fuck you cancer."
I guess I did not want to write this because I did not want cancer thinking we are having a tough time fighting. But you are right to ask me to share this. You have joined the fight against cancer if you are reading this, and I know that you can handle the truth. Just remember that in every fight - no matter how costly or how lengthy or how horrific - there is a victor. And cancer will not stand victorious after these battles. No way, no how.
Wednesday, September 14, 2011
Winning, duh!
I am in Houston to start the second part of the clinical trial. This is exactly like the last week of the the first part - high-dose InterLeukin II. I won't have the side effects of the TIL (tumor infiltrating lymphocytes) treatment that kicked off my last stay in the hospital so my infant immune system should not keep me in the hospital any prolonged period of time this stay, and I hope to head home by the middle of next week. Interestingly enough, the doctors say that the the IL2 this time is actually worse without the TIL.
Today I met with the head of the MD Anderson melanoma department, Dr. Hwu, who is also the head of the clinical trial I am going through. I asked him what else I can do to help the t-cells kick cancer's ass after I get home from the hospital. He said that anything helping my immune system recover and grow is a help. I've already addressed that with a plant-based ph-level diet and excercise, as well as avoiding snotty-nosed kids (except mine). He mentioned a blind study that compared the success rates of patients who participated in creative writing and those who did not. The conclusions were that patients involved in actively expressing themselves had higher response rates. He suggested any process of removing stress from meditation to yoga to writing. Maybe I'm not writing a blog, maybe I'm actually healing myself!
Of course, this all seems a little bit obvious to me. I firmly believe that what we think translates directly into what we are. An important part of that is what we choose to focus on. Our mind, like a camera lens, can make things sharp or fuzzy; big or small. And we have our fingers on the lens controls, no one else does. So when the doctor suggested trying to not take it all in too much, to not be too burdened too much by all of this, it resonated with me. Indeed I see this as the source of my strength through this struggle. Fighting cancer can seem overwhelming and all intrusive. It can seem that all of my life is involved with cancer and nothing of my old life is left, that it occupies every last corner. But instead I choose to see the battle against cancer in fragments. There are doctor visits here and there, occaisional pin pricks and IVs, random and unexplained pains that come and go like the winds. Certainly there have been alot of them, but I choose to see them as interuptions along the walk of a wonderful life.
And it works the other way, too. What I do choose to see as overwhelming and pervasive is the amount of care, love and warmth that has come my way as I have gone to fight this battle. Every day brings another surprise, another level of unselfish caring. Aquaintences, not familiar enough to even call friends, reaching out beyond their comfort zones to be sure that I am OK and offer any assistance they can. Family members, long since considered close, have flown back in to support their own. Medical professionals, to whom I should only be a medical ID number, have grown fond of the stories of my children and express an investment in my recovery that belies sincere concern. This is everywhere in my life, it is entirely inescapable.
One caring group, not only caring for me but also for my baby steps I've made in getting a message out about the misconceptions of skin cancer amongst the young and healthy, is zMotion. They have allowed me to participate in their promotion of the LiveLong LiveStrong even this October and offer continued support. As a matter of fact, Zimmerman advertising agency which sponsors zMotion cycling, just finished a video promoting the event that shares my story (you can see it here). Ann is still raising funds for LiveStrong and this event. I have a new batch of my special cancer fighting bracelets in and I'll send you one if you donate to LiveStrong at her site (here).
So maybe I'm a little crazy to think that it seems obvious. Maybe I'm delusional to think the recomendations of doctors seem straightforward enough to be simplistic. Maybe I'm a little nuts to expect to kick cancer's ass. It's not that I'm taking anything for granted, believe me I am not, I'm appreciating the great magnitude of all the forces being brought to this battle. That support becomes the troops, the reinforcements, the logistical bases, the high-tech weaponry. From friends to medical experts to anonymous supporters, the forces aligned against cancer in this war are awesome to behold. Cancer has picked the wrong fight this time, chosen the wrong body. Cancer is going to pay for that mistake, and not just in my body now. The message going out just may prevent cancer from forming a beach-hold somewhere else. Winning.
Today I met with the head of the MD Anderson melanoma department, Dr. Hwu, who is also the head of the clinical trial I am going through. I asked him what else I can do to help the t-cells kick cancer's ass after I get home from the hospital. He said that anything helping my immune system recover and grow is a help. I've already addressed that with a plant-based ph-level diet and excercise, as well as avoiding snotty-nosed kids (except mine). He mentioned a blind study that compared the success rates of patients who participated in creative writing and those who did not. The conclusions were that patients involved in actively expressing themselves had higher response rates. He suggested any process of removing stress from meditation to yoga to writing. Maybe I'm not writing a blog, maybe I'm actually healing myself!
Of course, this all seems a little bit obvious to me. I firmly believe that what we think translates directly into what we are. An important part of that is what we choose to focus on. Our mind, like a camera lens, can make things sharp or fuzzy; big or small. And we have our fingers on the lens controls, no one else does. So when the doctor suggested trying to not take it all in too much, to not be too burdened too much by all of this, it resonated with me. Indeed I see this as the source of my strength through this struggle. Fighting cancer can seem overwhelming and all intrusive. It can seem that all of my life is involved with cancer and nothing of my old life is left, that it occupies every last corner. But instead I choose to see the battle against cancer in fragments. There are doctor visits here and there, occaisional pin pricks and IVs, random and unexplained pains that come and go like the winds. Certainly there have been alot of them, but I choose to see them as interuptions along the walk of a wonderful life.
And it works the other way, too. What I do choose to see as overwhelming and pervasive is the amount of care, love and warmth that has come my way as I have gone to fight this battle. Every day brings another surprise, another level of unselfish caring. Aquaintences, not familiar enough to even call friends, reaching out beyond their comfort zones to be sure that I am OK and offer any assistance they can. Family members, long since considered close, have flown back in to support their own. Medical professionals, to whom I should only be a medical ID number, have grown fond of the stories of my children and express an investment in my recovery that belies sincere concern. This is everywhere in my life, it is entirely inescapable.
One caring group, not only caring for me but also for my baby steps I've made in getting a message out about the misconceptions of skin cancer amongst the young and healthy, is zMotion. They have allowed me to participate in their promotion of the LiveLong LiveStrong even this October and offer continued support. As a matter of fact, Zimmerman advertising agency which sponsors zMotion cycling, just finished a video promoting the event that shares my story (you can see it here). Ann is still raising funds for LiveStrong and this event. I have a new batch of my special cancer fighting bracelets in and I'll send you one if you donate to LiveStrong at her site (here).
So maybe I'm a little crazy to think that it seems obvious. Maybe I'm delusional to think the recomendations of doctors seem straightforward enough to be simplistic. Maybe I'm a little nuts to expect to kick cancer's ass. It's not that I'm taking anything for granted, believe me I am not, I'm appreciating the great magnitude of all the forces being brought to this battle. That support becomes the troops, the reinforcements, the logistical bases, the high-tech weaponry. From friends to medical experts to anonymous supporters, the forces aligned against cancer in this war are awesome to behold. Cancer has picked the wrong fight this time, chosen the wrong body. Cancer is going to pay for that mistake, and not just in my body now. The message going out just may prevent cancer from forming a beach-hold somewhere else. Winning.
Monday, September 5, 2011
Fighting Words
I’ve been home for a few days now and I’m feeling very much alive. The new t-cells must be working as there has been 'sensitivity' around the areas of my metastasis, and some have visually shrunk already. I’m pretty restricted in pain medication options because of the sensitivity of my immune system and the antibiotics I’m taking, so I’m toughing it out old school. I know that a few bad days will help me appreciate the good ones.
Mentally it has been a few good days at home. When I left the hospital last Thursday I felt something transformational, like a weight off my shoulders or some line crossed underneath my feet. My confidence level ticked up a notch and I now feel really good about my chances from here on out. Statistically I have moved into a select subset of those fighting late-stage melanoma of which a majority expects positive long-term response. It’s the first time since this fight started that I’m on the business side of 50% - and it feels very good to be here.
Although "here" can be a bit lonely as I do not have many friends who are battling cancer. This is probably because of the distance I am traveling to receive my treatment, or more honestly, my reluctance to reach out to other survivors. One friend I do have is a young woman with three small children, a job and stage 4 melanoma very much like mine. Her blog inspired mine and, although we've never met, we e-mail at length about the many tough and the sometimes humorous sides of facing cancer. We wrestle with many of the same treatment decisions, sometimes with the same medical teams. We also confide some darker thoughts to each other about dealing with oblivious healthy people and self-centered care givers, cancer insider stuff. On Thursday, as I skipped out of the front doors of MD Anderson resplendent in my newfound confidence, on the other side of Texas my friend lost her battle with melanoma. Irrespective of my oft-quoted Mr. Churchill, failure is indeed sometimes fatal.
This blow - and it is a surprisingly painful one - serves to underscore the seriousness of my endeavor, our battle. And I choose those militant terms quite deliberately. The NY Times on Sunday examined the debated use of militant terms to describe dealing with cancer. People such as Dr. Andrew Weill suggest it is more healthy to see cancer as part of the natural process, a problem that needs to be solved rationally. That calling cancer an "enemy" is more self victimizing and less calming. They also suggest that militant speak makes “losers” out of, well, losers. Dr. Weill and his type can kiss my tumor-riddled ass. My friend did not die and leave her family behind because of a health issue poorly considered. She is not a “loser” in that she lost what she saw was a battle for her life. Cancer is evil, it is an enemy that wants to take the ultimate property away from us, our bodies. What it may lack in obvious intelligence it makes up for in deadly persistence. And like any horrible foe, it is ultimately conquerable and hopefully it will be eradicated in my time. In that time, like my friend, I am going to fight and fight and fight. I am not going to honor cancer by calling it a natural process. I am not going to limit my response to the rational. I am not going to thank God for the bluebird singing outside my hospital room window. I am going to force cancer into a corner and then I’m going to strangle the life out of it. I’ll be thinking of my friend when I do.
Friday, September 2, 2011
RTB - return to base
To update, the t-cell replacement phase of the clinical trial is over and I am back home. Nothing like 16 days in the hospital to make you appreciate the finer points of the ole homestead. In those 16 days we killed off my immune system with chemo, replaced that with my newly grown t-cells designed to fight melanoma, used high-dose IL2 to welcome and grow the new t-cells and then waited for immune system to bounce back enough to let me out in the general population with you germ infested types. The chemo went by pretty easily, although the after effects are just starting to be felt. As of today I am severely follicly challenged.
The t-cell transfer was exciting, albeit a little anticlimactic. Two scientists brought the bag of t-cells to the research team, who handed them to my medical oncologist, who handed it to the clinical nurses who handed it to my day's nurse. In thirty minutes they were in, all the while all the aforementioned medical staff loitered around my tiny hospital room. I'm officially the 46th person to have undergone this at MD Anderson (about 100 have undergone it at the National Cancer Institute). They have done surgery on nearly 500 patients at MD A in order to get them into the study but most of them dropped out along the way. Not me, this was my plan from day #1 and - much to the misfortune of cancer - I succeeded. One thing that I noticed in the hospital is that there were two types of patients - those having things done to them and those having things done for them. It comes out in the way people describe their treatment, being subjugated or being empowered. My chosen medical team has performed some major science fiction for me in my battle for cancer, I can not thank them enough. Here is a picture of me with Dr. Patrick Hwu, who developed this process with the famous Dr. Rosenburg when they used to work together at NCI (I promise that is him). I go back on 9/13 for another round of high-dose IL2. I have to say that the HDIL2 is pretty rough, but the effects seem to be short lived. I had five doses last week, and hope for at least as many when I go back. Then we have an initial set of scans at six weeks and twelve weeks. My treatment protocol is complete at this point, and it will be time to get back to work and a normal life.
Speaking of getting to work, kudos to my wife Ann who is riding in the LiveLong/LiveStrong event on October 2nd and she's the third highest contributor so far for the organization, in addition to getting quite a few friends and neighbors to participate in the ride. If you want to participate or support Ann, she has a dedicated web page with all the information here. I am very excited about the ride, and plan on riding one of the three courses, even if I'm in a wagon being pulled by zMotion riders.
Yesterday I was in the hospital hooked up to Wilson and a dozen other machines, being poked and prodded around the clock. This morning I lay in bed with a little girl in each arm watching the sun rise over the hedges. The war is not over, not by a long shot, but it is good to be home to savor a victory.
"Success is not final, failure is not fatal; it is the courage to continue that counts." W. Churchill
Tuesday, August 23, 2011
Cone of Uncertainty
I've finished a week of lymphodepletion here in Houston and I am scheduled to get my new t-cells tomorrow afternoon. The hospital staff and medical team are all abuzz about my looming Day 0. My white blood cell count was 0.8 this morning, down from over 8.0 when I checked in (normal levels are 4.0 - 11.0). They should be 0.0 by tomorrow and I had my last chemo round this morning. The chemo has not been that bad. The first two days of cyclophosphamide were pretty bad in terms of the nausea and chemo brain. But the last five doses of fludarabine have had little impact on my physical or mental faculties. They have even cut me loose from the IV pole for dinner the past couple of nights which has been wonderful. Besides those respites, me and that IV pole are literally inseparable. I spend all day with it, sleep with it, take it to the bathroom with me. It reminds me of my M16 rifle at Parris Island. I actually caught myself arguing with it the other day when it was beeping at me saying it needed to be plugged in to recharge it's batteries. I knew It had another hour or so in reserve. However, Wilson - that's what he likes to be called - won the argument. He always does, and why wouldn't he with that infuriating beeping?
To keep from going nuts I am employing the techniques I've learned from many television seasons of "Lock Up" and "Locked Up Abroad" on TV. I exercise every morning, schedule my in-room breakfast followed by coffee with my Dad. I spend my afternoons in the observatory on the 24th floor playing video games or writing poetry. I started a series I call "hospitalization haikus". My first is an observation on Wilson:
Hanging icicle drips
Poison, melting, drip by drip.
In spring hope explodes.
I have many more. Right now I am adjusting to isolation, which started this morning. Because they killed off all of my white blood cells I am prone to catch any little virus I come into contact with. Everyone who comes into contact with me needs to wear masks and gloves, even my dad sitting in the room watching TV with me. I can still leave the hospital room for one more day, as long as I wear the same garb. So I haunt the hospital floors looking like a surgeon in pajamas. After tomorrow I'll be in lockdown when they introduce the new t-cells and start the high dose IL2. Then we wait at least five, or as many as fifteen, days until my white blood cell counts get back up to an acceptable level. Of course, I'm expecting to be on the short side of that based on my previous bounce back from biochemotherapy. Either way, I'm going to be here for a while. I don't even dare to start thinking about going home. But it has been especially difficult being here with hurricane Irene threatening home the past few days. This morning they moved south Florida out of the "cone of uncertainty" for hurricane Irene. I'm glad the wife and kids and grandma and the dogs do not need to deal with an evacuation, nor do all the other residents so familiar with hurricane's death and destruction. It looks like my situation with the cell transfer has also finally moved out of the cone of uncertainty. Perhaps I am in the sphere of possibility, or the cube of positivity. Whatever we call it, a close call with potential disaster has been averted for now both here and there. Although I am far from home I know what I've missed with the family in these weeks will be paid back a million-fold when this works. And it's a good place to be here with Wilson and the great MD Anderson medical team, kicking cancer's ass around the clock, non-stop, 24/7.
To keep from going nuts I am employing the techniques I've learned from many television seasons of "Lock Up" and "Locked Up Abroad" on TV. I exercise every morning, schedule my in-room breakfast followed by coffee with my Dad. I spend my afternoons in the observatory on the 24th floor playing video games or writing poetry. I started a series I call "hospitalization haikus". My first is an observation on Wilson:
Hanging icicle drips
Poison, melting, drip by drip.
In spring hope explodes.
I have many more. Right now I am adjusting to isolation, which started this morning. Because they killed off all of my white blood cells I am prone to catch any little virus I come into contact with. Everyone who comes into contact with me needs to wear masks and gloves, even my dad sitting in the room watching TV with me. I can still leave the hospital room for one more day, as long as I wear the same garb. So I haunt the hospital floors looking like a surgeon in pajamas. After tomorrow I'll be in lockdown when they introduce the new t-cells and start the high dose IL2. Then we wait at least five, or as many as fifteen, days until my white blood cell counts get back up to an acceptable level. Of course, I'm expecting to be on the short side of that based on my previous bounce back from biochemotherapy. Either way, I'm going to be here for a while. I don't even dare to start thinking about going home. But it has been especially difficult being here with hurricane Irene threatening home the past few days. This morning they moved south Florida out of the "cone of uncertainty" for hurricane Irene. I'm glad the wife and kids and grandma and the dogs do not need to deal with an evacuation, nor do all the other residents so familiar with hurricane's death and destruction. It looks like my situation with the cell transfer has also finally moved out of the cone of uncertainty. Perhaps I am in the sphere of possibility, or the cube of positivity. Whatever we call it, a close call with potential disaster has been averted for now both here and there. Although I am far from home I know what I've missed with the family in these weeks will be paid back a million-fold when this works. And it's a good place to be here with Wilson and the great MD Anderson medical team, kicking cancer's ass around the clock, non-stop, 24/7.
Tuesday, August 16, 2011
Game On
Well, I am in the hospital room at MD Anderson right now and ready to start the adoptive cell therapy tomorrow. Then it's game on. I feel really strong right now, although cancer has gotten a few licks in over the past couple of weeks. The tumor in my head has been hurting and the one near my liver feels like someone is constantly elbowing me in the back, along with the other annoying aches and pains. Dick Marcinko says pain is a positive signal, proof positive that you are still alive. A lot of pain makes you "VMA" - very much alive. I think cancer is really scared and is just throwing in some jabs before the real showdown. It will take more than a headache and a poke in the ribs to scare me off. In fact, it's really serving to piss me off. I've been getting really angry waiting for this clinical trial. Angry that cancer sucks so bad. Angry that cancer affects 28 million people around the world. Angry that we haven't beaten in yet. Angry that so few people know enough about it to care. But I welcome the anger, it is the fuel for toughness.
 If I needed a lesson in toughness this week I got one from my five year old. She sprained her neck the other morning before school. Our chiropractor friend adjusted her before she went to school but she was still pretty sore and held her head at a twenty degree list all day. She insisted on going to her last day of pre-kindergarten and to her karate class. The first was fun and not physically challenging, but I was willing to let her slide on the martial arts. She knows the importance of showing up for karate class unless absolutely unavoidable. To not show up is an insult to the teacher and to the martial arts school. This a lesson they teach the students on day one. So she uniformed up and went through the whole class without complaint. At one point the sensai noticed her stiff neck and pulled her out of the wrestling-with-classmates portion of the class. Instead, he chose to be her wrestling opponent for a class demonstration. She won the match, giggling all the way. When I expressed to her how proud I was of her for going to the class when she could have stayed home she said that, like Horton in the Dr. Seuss story we read the night before, she had to do "the right thing." Amazing. Inspiring.
If I needed a lesson in toughness this week I got one from my five year old. She sprained her neck the other morning before school. Our chiropractor friend adjusted her before she went to school but she was still pretty sore and held her head at a twenty degree list all day. She insisted on going to her last day of pre-kindergarten and to her karate class. The first was fun and not physically challenging, but I was willing to let her slide on the martial arts. She knows the importance of showing up for karate class unless absolutely unavoidable. To not show up is an insult to the teacher and to the martial arts school. This a lesson they teach the students on day one. So she uniformed up and went through the whole class without complaint. At one point the sensai noticed her stiff neck and pulled her out of the wrestling-with-classmates portion of the class. Instead, he chose to be her wrestling opponent for a class demonstration. She won the match, giggling all the way. When I expressed to her how proud I was of her for going to the class when she could have stayed home she said that, like Horton in the Dr. Seuss story we read the night before, she had to do "the right thing." Amazing. Inspiring.
Well, I plan on seeing her earn her next belt in karate. I plan on seeing her get her blackbelt. I plan on seeing more of her doing the right thing as she grows up. Now it's my turn to do the right thing. My turn to tough it out and show up for the fight with this cancer that threatens to take away all of that. My turn to step up, suck it up and harden the fuck up. It's time to fight.
It's on, cancer. You and me, tomorrow. And I'm going to kick your ass.
 If I needed a lesson in toughness this week I got one from my five year old. She sprained her neck the other morning before school. Our chiropractor friend adjusted her before she went to school but she was still pretty sore and held her head at a twenty degree list all day. She insisted on going to her last day of pre-kindergarten and to her karate class. The first was fun and not physically challenging, but I was willing to let her slide on the martial arts. She knows the importance of showing up for karate class unless absolutely unavoidable. To not show up is an insult to the teacher and to the martial arts school. This a lesson they teach the students on day one. So she uniformed up and went through the whole class without complaint. At one point the sensai noticed her stiff neck and pulled her out of the wrestling-with-classmates portion of the class. Instead, he chose to be her wrestling opponent for a class demonstration. She won the match, giggling all the way. When I expressed to her how proud I was of her for going to the class when she could have stayed home she said that, like Horton in the Dr. Seuss story we read the night before, she had to do "the right thing." Amazing. Inspiring.
If I needed a lesson in toughness this week I got one from my five year old. She sprained her neck the other morning before school. Our chiropractor friend adjusted her before she went to school but she was still pretty sore and held her head at a twenty degree list all day. She insisted on going to her last day of pre-kindergarten and to her karate class. The first was fun and not physically challenging, but I was willing to let her slide on the martial arts. She knows the importance of showing up for karate class unless absolutely unavoidable. To not show up is an insult to the teacher and to the martial arts school. This a lesson they teach the students on day one. So she uniformed up and went through the whole class without complaint. At one point the sensai noticed her stiff neck and pulled her out of the wrestling-with-classmates portion of the class. Instead, he chose to be her wrestling opponent for a class demonstration. She won the match, giggling all the way. When I expressed to her how proud I was of her for going to the class when she could have stayed home she said that, like Horton in the Dr. Seuss story we read the night before, she had to do "the right thing." Amazing. Inspiring. Well, I plan on seeing her earn her next belt in karate. I plan on seeing her get her blackbelt. I plan on seeing more of her doing the right thing as she grows up. Now it's my turn to do the right thing. My turn to tough it out and show up for the fight with this cancer that threatens to take away all of that. My turn to step up, suck it up and harden the fuck up. It's time to fight.
It's on, cancer. You and me, tomorrow. And I'm going to kick your ass.
Wednesday, August 3, 2011
Count Down to T-Day
We have a schedule for the TIL treatment, and I go to Texas on August 15th for two weeks. I’m not sure if “excited” is the word but I am psyched about the promising results and the cutting edge science. The week of waiting for the date was nerve racking because my whole plan on getting this trial done before my medical leave of absence expires depends on timely scheduling. When the doctors don’t call you back you inevitably start coming up with reasons why. So I had one wonderful day of knowing the date was set in stone. Then I got a call from the TIL team asking to get a rush job brain MRI before they thaw out my t-cells on August 8th. They are concerned about cancer activity in my brain because of the other metastasis within my skull. I have a cranium lesion, orbital metastasis and – as of June 30th - an intercranial metastasis, but still no brain tumor. A brain tumor would exclude me from the TIL study, at least until it was treated. Not quite an “oh, shit!” moment, but definitely a rapid dissipation of a too-short lived relatively good feeling. I’m fond of saying (at least from now on) that the deal is not done until the needle is in your arm, and maybe not even then.
The interesting thing about that call, and I’ve noticed this more and more lately, is the sharp contrast between the routine manner of communicating such news and the life changing affect it can potentially have on the receiver. As occasionally in life when something drastic happens to us and we have to deal with someone to whom the event is routine. Like getting in a car accident or getting mugged. Your life seems turned upside down, the impact seems severe with possible long-term effects but the police officer taking the report sees it everyday. You can feel the same vibe from the oncologists and nurses, they know the stats and what seems to you as devastating is to them routine. I guess after a while one’s definition of routine can change, but I now understand why cancer patients and their caregivers can suffer from Post Traumatic Stress Disorder. It can seem, at times, overwhelming.
But, of course, we will not let this hold us back. It has been said that worry does not empty tomorrow of its sorrow, it empties today of its strength. I’ll assume everything is on track for my immune system upgrade to 2.0, special melanoma fighting edition. I’ve been on the stationary bike and hitting the weights. I’ve been vegan for over a week, boosting my immune system. My caregivers are lined up and the flights have been booked. I’m going in strong, chin down and elbows in – swinging. Watch out cancer, it’s almost time to meet my version of the Green Berets.
The interesting thing about that call, and I’ve noticed this more and more lately, is the sharp contrast between the routine manner of communicating such news and the life changing affect it can potentially have on the receiver. As occasionally in life when something drastic happens to us and we have to deal with someone to whom the event is routine. Like getting in a car accident or getting mugged. Your life seems turned upside down, the impact seems severe with possible long-term effects but the police officer taking the report sees it everyday. You can feel the same vibe from the oncologists and nurses, they know the stats and what seems to you as devastating is to them routine. I guess after a while one’s definition of routine can change, but I now understand why cancer patients and their caregivers can suffer from Post Traumatic Stress Disorder. It can seem, at times, overwhelming.
But, of course, we will not let this hold us back. It has been said that worry does not empty tomorrow of its sorrow, it empties today of its strength. I’ll assume everything is on track for my immune system upgrade to 2.0, special melanoma fighting edition. I’ve been on the stationary bike and hitting the weights. I’ve been vegan for over a week, boosting my immune system. My caregivers are lined up and the flights have been booked. I’m going in strong, chin down and elbows in – swinging. Watch out cancer, it’s almost time to meet my version of the Green Berets.
Thursday, July 28, 2011
Update - sort of
With the end of the Tour de France and my ongoing wait for a spot in the clinical trial, I thought I would take time to catch you up with a random collection of facts and observations I have not been able to tie into any narrative thread, but feel important to share.
• I've recently adopted a very short haircut, in part to externalize my fighting spirit and partly to cover up the result of radiation therapy. Thankfully, my hair did not fall out from the chemotherapy. However, it did disappear along the side of my head where the radiation beam went through my eye socket and continued on to China. So I wear my hair short these days waiting for the hair to return (fingers crossed). If I let it grow, I look exactly like this guy from the toilet paper commercial.
• My only other obvious sign of therapy has been my right eye. The tumor there has ceased to cause blind spots but still limits my near vision significantly. My left eye can read fine. As the degree of this is still fluctuating I am hesitant to order another pair of soon-to-be useless glasses and have opted for store-bought reading glasses. My recent solution is to buy a strong prescription strength pair and pop out the left lens. It gives me an intellectual homeless look and helps keep the seat next to me empty on airplanes.
• I have been shuttling between Ft. Lauderdale and Houston on Southwest Airlines, which has a couple direct flights a day and no change fees (important when you have those open-ended doctor appointments). Last week I was elevated to their “A-list” category because of my frequent flying. I now have the highest status on the cheapest, no-frills airline in the country. Yeah! Not exactly like George Clooney’s character in “Up in the Air”, but two bags of peanuts are always better than one.
• Food tastes have largely bounced back from chemotherapy. Before treatment I classified food into three categories – unacceptable, acceptable and enjoyable. The split was roughly 15/60/25% and after treatment it was 15%/84%/1%. My love of everything coffee related took a real hit, as I could not stomach it in any version. This was especially painful after my significant purchase earlier this year of a gleaming chrome and black Swiss designed, Italian espresso machine. I can now drink coffees and lungos and lattes, but the love has yet to return. However, not having to wake up for anything seems to counterbalance this somewhat. Ann and I have recently started eating raw vegan from previously eating a vegetarian diet. This makes the food split about 98%/1%/1%.
• Appetite is one of the common casualties of chemotherapy, which leads to inevitable weight loss. This is so cruel as it is one point in your life that you want and need to gain weight but when you have lost any taste for food. Note that cancer research has shown that the chemical marinol is one of the most effective anti-nausea appetite-building drugs available. It occurs naturally in cannabis sativa (marijuana). Just saying.
• Those of you who know me know that only alcohol can beat out coffee in terms of most likely to be in my hand at any given time. This went out the window during the first treatment, partially from recommendations of the medical team but mostly from taste. Now I can stomach a hoppy wheat beer with a meal but no wine or other alcohol. Besides the obvious physiological improvements that resulted I estimate this has saved me between $50 and $350 a week. Who said cancer treatment does not have a positive side?
• Other positives include the skin rejuvenation I received on my last round of chemotherapy. My face peeled non-stop for almost three weeks. As a result, I still have people telling me how much younger I look. Laser skin resurfacing costs an average of $2,100 according to Dr. Oz. In addition to significant costs savings from dry cleaning, hair products, commuting costs of gas and tolls, I think I may be in for a financial windfall.
• Among the things I’ve been spending my new found wealth on are my own version of the LiveStrong yellow wristbands. Yes, I sport the LiveStrong band and will get a LiveStrong tattoo once I kick this thing. It is one of the most effective organizations to support patients and raise cancer awareness. While I do not want to try to improve on perfection, the LiveStrong band is just a little polite for my own version of a campaign against the disease. I wanted something that captures the magnitude of struggle and deep emotional connection that I feel to it. So I have created my own wristband that me and my friends are sporting that is a little more on point. Let me know if you want one. Get one for grandma, too, but please note that they do not come in kid sizes.
• My wife has used some of the money to pamper me in my time of need. She does, however, get the least usable present award for buying me a gift certificate for a scalp massage after receiving a particularly fabulous one at a local spa. A few days later we found out I had a skull lesion, basically a hole in my head that is probably best not massaged. Awkward. But this did not stop her from the requisite “hole in the head” comments.
• Ann, of course, has been my champion through all of this. We laugh, we cry – but mostly we laugh. That’s why I love her and why I married her. We know that many cancer books recommend latching onto a poem or a song that can help pull you through the tough times. We could not get past a rewording of John Denver’s “Sunshine” where “sunshine on my shoulders makes me happy” becomes “sunshine on my shoulders gives me cancer” (my first and second incidents of melanoma were on my left shoulder). OK, you probably had to be there for that.
• Another inside joke between us stemmed from the award winning biggest understatement of a nurse who, upon checking off my list of symptoms, stated that I was in “perfect health – well, except for the cancer.” Now Ann I use this as our standard line when we so often have to go through these checklists. We tell them “no nausea, no pain, no falling or injuries, etc., etc., – I’m in perfect health”, then - in unison - “except for the cancer!” [buh-bump]. Cracks me up everytime, but many nurses seem have no sense of humor. I don’t think cancer has a sense of humor either.
• I've recently adopted a very short haircut, in part to externalize my fighting spirit and partly to cover up the result of radiation therapy. Thankfully, my hair did not fall out from the chemotherapy. However, it did disappear along the side of my head where the radiation beam went through my eye socket and continued on to China. So I wear my hair short these days waiting for the hair to return (fingers crossed). If I let it grow, I look exactly like this guy from the toilet paper commercial.
• My only other obvious sign of therapy has been my right eye. The tumor there has ceased to cause blind spots but still limits my near vision significantly. My left eye can read fine. As the degree of this is still fluctuating I am hesitant to order another pair of soon-to-be useless glasses and have opted for store-bought reading glasses. My recent solution is to buy a strong prescription strength pair and pop out the left lens. It gives me an intellectual homeless look and helps keep the seat next to me empty on airplanes.
• I have been shuttling between Ft. Lauderdale and Houston on Southwest Airlines, which has a couple direct flights a day and no change fees (important when you have those open-ended doctor appointments). Last week I was elevated to their “A-list” category because of my frequent flying. I now have the highest status on the cheapest, no-frills airline in the country. Yeah! Not exactly like George Clooney’s character in “Up in the Air”, but two bags of peanuts are always better than one.
• Food tastes have largely bounced back from chemotherapy. Before treatment I classified food into three categories – unacceptable, acceptable and enjoyable. The split was roughly 15/60/25% and after treatment it was 15%/84%/1%. My love of everything coffee related took a real hit, as I could not stomach it in any version. This was especially painful after my significant purchase earlier this year of a gleaming chrome and black Swiss designed, Italian espresso machine. I can now drink coffees and lungos and lattes, but the love has yet to return. However, not having to wake up for anything seems to counterbalance this somewhat. Ann and I have recently started eating raw vegan from previously eating a vegetarian diet. This makes the food split about 98%/1%/1%.
• Appetite is one of the common casualties of chemotherapy, which leads to inevitable weight loss. This is so cruel as it is one point in your life that you want and need to gain weight but when you have lost any taste for food. Note that cancer research has shown that the chemical marinol is one of the most effective anti-nausea appetite-building drugs available. It occurs naturally in cannabis sativa (marijuana). Just saying.
• Those of you who know me know that only alcohol can beat out coffee in terms of most likely to be in my hand at any given time. This went out the window during the first treatment, partially from recommendations of the medical team but mostly from taste. Now I can stomach a hoppy wheat beer with a meal but no wine or other alcohol. Besides the obvious physiological improvements that resulted I estimate this has saved me between $50 and $350 a week. Who said cancer treatment does not have a positive side?
• Other positives include the skin rejuvenation I received on my last round of chemotherapy. My face peeled non-stop for almost three weeks. As a result, I still have people telling me how much younger I look. Laser skin resurfacing costs an average of $2,100 according to Dr. Oz. In addition to significant costs savings from dry cleaning, hair products, commuting costs of gas and tolls, I think I may be in for a financial windfall.
• Among the things I’ve been spending my new found wealth on are my own version of the LiveStrong yellow wristbands. Yes, I sport the LiveStrong band and will get a LiveStrong tattoo once I kick this thing. It is one of the most effective organizations to support patients and raise cancer awareness. While I do not want to try to improve on perfection, the LiveStrong band is just a little polite for my own version of a campaign against the disease. I wanted something that captures the magnitude of struggle and deep emotional connection that I feel to it. So I have created my own wristband that me and my friends are sporting that is a little more on point. Let me know if you want one. Get one for grandma, too, but please note that they do not come in kid sizes.
• My wife has used some of the money to pamper me in my time of need. She does, however, get the least usable present award for buying me a gift certificate for a scalp massage after receiving a particularly fabulous one at a local spa. A few days later we found out I had a skull lesion, basically a hole in my head that is probably best not massaged. Awkward. But this did not stop her from the requisite “hole in the head” comments.
• Ann, of course, has been my champion through all of this. We laugh, we cry – but mostly we laugh. That’s why I love her and why I married her. We know that many cancer books recommend latching onto a poem or a song that can help pull you through the tough times. We could not get past a rewording of John Denver’s “Sunshine” where “sunshine on my shoulders makes me happy” becomes “sunshine on my shoulders gives me cancer” (my first and second incidents of melanoma were on my left shoulder). OK, you probably had to be there for that.
• Another inside joke between us stemmed from the award winning biggest understatement of a nurse who, upon checking off my list of symptoms, stated that I was in “perfect health – well, except for the cancer.” Now Ann I use this as our standard line when we so often have to go through these checklists. We tell them “no nausea, no pain, no falling or injuries, etc., etc., – I’m in perfect health”, then - in unison - “except for the cancer!” [buh-bump]. Cracks me up everytime, but many nurses seem have no sense of humor. I don’t think cancer has a sense of humor either.
Saturday, July 23, 2011
Odds
Good news on the TIL clinical trial, my insurance company has come on board to pay their share of the costs. It took a lot of phone calls and explanations about the trial but they ponied up for a sizable portion of the very sizable costs (the sponsoring drug company pays much of the rest). If I bothered to see if Cigna or Novartis had a Facebook page I'd ask you to friend them. So with that out of the way I anticipated a rapid entry to the study but I found out this week about a potentially devastating delay, one that quite literally would be decided by a roll of the dice. This clinical trial has two arms, one is standard TIL and the other is standard TIL plus an experimental vaccine. Patients are randomized into each arm equally, giving patients a 50% chance to get in one arm or the other. This helps the researchers determine statistically if one arm has different results than the other, a standard part of any trial. The past few patients for this trial have been randomized into the vaccine arm which carries with it a few extra weeks of delay to prepare the extra vaccine. Given that they can process only two patients a month in the trial, the vaccine delay and the length of the TIL procedure, that means a new entrant into the vaccine arm would be lucky to start the trial in September or October. If that happened to me then it would mean being in treatment when my medical leave of absence from work runs out. That means the end of my job. That means the end of my benefits. Good feeling rapidly gone. So today I went to MD Anderson to roll the dice. Its actually done on a computer, but I think they should make some kind of fancy lit-up roulette wheel since they dragged me all the way to Texas to do this. But the roll came up in my favor, the non-vaccine study. Dr. Patel is trying to start me in the study in the first week of August. That may be delayed slightly, but unlikely long enough to complicate my work plans. Sometimes things just work out.
I recently started reading Evan Handler's "It's Only Temporary", an honest and often hilarious tale of leukemia survival (yes, you read that correctly). Evan writes about facing down 50% odds of survival and how the gravity of that impacted him and the lives of his friends and family. It put my view of being overjoyed about the TIL study, that may give me a 50% chance of response, in contrast. I'm ten months into the median 12 months survival for melanoma patients, facing down an 85% chance of not seeing the 2015 Tour de France (and George Hincapie's 20th participation). Unlike Evan Handler, I don't have a statistically significant chance of dying - I have a statistically insignificant chance of living.
I've actually been digging into all these statistics recently. In part because of my involvement in Florida's first LiveStrong event on October first and second. z-Motion, the riding club I belong to and strong community supporter, is a primary sponsor of the event. It will include rides and runs and walks to raise money for the Livestrong foundation and increase awareness of cancer. I hope to ride in the event which occurs on the date Lance Armstrong was diagnosed with cancer. Since my doctors approved me riding a stationary bike a few weeks ago I have been training and increasing my workload every day. Last week I rode a 100 miles, this week 66 miles so far at an average 220 watts. I would be relatively happy with those numbers before I got sick. Through z-Motion I'm trying to use the story of my diagnosis to help attract more attention and support for the event. I will also be speaking at a z-Motion gathering in August if I'm out of treatment. Outdoor athletes like z-Motion racers and riders are at higher risk of getting melanoma and also have a lower probability of early detection than the average populace. Its counterintuitive that a healthy lifestyle can increase cancer risks, and that's my message - my hook. When I tell people about melanoma I want to be accurate, so I researched the latest grim stats. Incidence of melanoma is increasing at a faster rate than any of the seven most common cancers. It is one of only three cancers with an increasing mortality rate in men. Its the number one cancer for twenty-five to twenty-nine year olds. Someone dies from melanoma in the US every 62 minutes. It claims more life years than any other cancer because it the average age of its victims is fifteen to twenty years younger than all other cancers. There is no cure.
Sobering thoughts like these usually drive me into attack mode, make me want to kill someone or something. Fight, fight, fight. Then fight some more. Yes, I know that someone has to be in those small percentages, and that is where I will be. Always have been, always will be. But sometimes the gravity, the seriousness, of it all comes over me like a water balloon rolling on to a pebble. We are, after all, not talking about a hand of poker or a bike race. I caught myself staring at otherworldly clouds outside the airplane window and wondering "what if?" I don't know what if's, but I do know that right now - 34,000 feet up in this aluminum tube - is as close to heaven as I ever want to get. Right now I want to get my feet on the ground and my arms around my little girls. I want to hold them really, really tight until I top up my suitcase of courage and can fight some more for them, because I know I'll fight much harder and longer for them than for myself. Cancer does not have small beautiful children to fight for. Cancer does not have decades of birthday parties to attend, prom photos to take, wedding aisles to walk daughters down. I do. In spades. And that's why I'm going to beat the odds. You can bet on it.
I recently started reading Evan Handler's "It's Only Temporary", an honest and often hilarious tale of leukemia survival (yes, you read that correctly). Evan writes about facing down 50% odds of survival and how the gravity of that impacted him and the lives of his friends and family. It put my view of being overjoyed about the TIL study, that may give me a 50% chance of response, in contrast. I'm ten months into the median 12 months survival for melanoma patients, facing down an 85% chance of not seeing the 2015 Tour de France (and George Hincapie's 20th participation). Unlike Evan Handler, I don't have a statistically significant chance of dying - I have a statistically insignificant chance of living.
I've actually been digging into all these statistics recently. In part because of my involvement in Florida's first LiveStrong event on October first and second. z-Motion, the riding club I belong to and strong community supporter, is a primary sponsor of the event. It will include rides and runs and walks to raise money for the Livestrong foundation and increase awareness of cancer. I hope to ride in the event which occurs on the date Lance Armstrong was diagnosed with cancer. Since my doctors approved me riding a stationary bike a few weeks ago I have been training and increasing my workload every day. Last week I rode a 100 miles, this week 66 miles so far at an average 220 watts. I would be relatively happy with those numbers before I got sick. Through z-Motion I'm trying to use the story of my diagnosis to help attract more attention and support for the event. I will also be speaking at a z-Motion gathering in August if I'm out of treatment. Outdoor athletes like z-Motion racers and riders are at higher risk of getting melanoma and also have a lower probability of early detection than the average populace. Its counterintuitive that a healthy lifestyle can increase cancer risks, and that's my message - my hook. When I tell people about melanoma I want to be accurate, so I researched the latest grim stats. Incidence of melanoma is increasing at a faster rate than any of the seven most common cancers. It is one of only three cancers with an increasing mortality rate in men. Its the number one cancer for twenty-five to twenty-nine year olds. Someone dies from melanoma in the US every 62 minutes. It claims more life years than any other cancer because it the average age of its victims is fifteen to twenty years younger than all other cancers. There is no cure.
Sobering thoughts like these usually drive me into attack mode, make me want to kill someone or something. Fight, fight, fight. Then fight some more. Yes, I know that someone has to be in those small percentages, and that is where I will be. Always have been, always will be. But sometimes the gravity, the seriousness, of it all comes over me like a water balloon rolling on to a pebble. We are, after all, not talking about a hand of poker or a bike race. I caught myself staring at otherworldly clouds outside the airplane window and wondering "what if?" I don't know what if's, but I do know that right now - 34,000 feet up in this aluminum tube - is as close to heaven as I ever want to get. Right now I want to get my feet on the ground and my arms around my little girls. I want to hold them really, really tight until I top up my suitcase of courage and can fight some more for them, because I know I'll fight much harder and longer for them than for myself. Cancer does not have small beautiful children to fight for. Cancer does not have decades of birthday parties to attend, prom photos to take, wedding aisles to walk daughters down. I do. In spades. And that's why I'm going to beat the odds. You can bet on it.
Friday, July 15, 2011
The Experts are Wrong (Sometimes)
“It's another fact of cancer that the more informed and empowered patient has a better chance of long-term survival.” Lance Armstrong
I’m not saying that I am not still making mistakes, but I always question assumptions – others and mine. The experience of cancer diagnosis is a scary one, more so than the actual treatment protocols. I've heard it described as being transported to another country. One day you are making coffee before work, taking your kids to school and planning your weekend. The next day after diagnosis you are alone in a foreign land where everybody speaks a different language. There are many people willing to help you, offering to show you the way home. But the path home is painted in the art of self reliance. That is the current state of cancer care, like it or not.
I’m by no means an expert in cancer diagnosis, but I’ve learned a few things from the experts and the so-called experts in the past year that have helped me avoid costly, perhaps life threatening mistakes. I feel that it is important to share these, because the most important lessons – as they often are in life – are the ones they do not put in books or brochures outside the doctor’s office. So sit back and join me on a journey through my diagnosis experience and see the lessons I have learned. They can literally save your life.
Experts have a hard time seeing beyond the focus of their expertise.
Many of the lessons I’ve learned deal with the fact that I am not, in medical terms, an “expert” and those that are considered experts are not always the right experts. This can sometimes be because of the question that you - the patient – are asking, either implicitly or explicitly. When I was starting to have mysterious black eyes on my right side I went immediately to an optometrist and then to an ophthalmologist. I was already assuming, implicitly by my selection of specialist, that something was wrong with my eye. These experts correctly told me that there was nothing wrong with my eye. They incorrectly told me that everything was probably OK, that my symptoms were some temporary isolated trauma that would go away soon. I took only their expert opinion about my eye and disregarded their other conclusion, as I knew it was an assumption beyond their expertise. The black eyes continued so I was right to disregard their sweeping statements of my good health.
Generalists can have a hard time looking beyond the obvious.
Assuming that my actual eye was OK I then went to my generalist doctor to see if there was something else that would explain the black eyes. He agreed with the specialist that it was some kind of local trauma and that the big picture – my excellent overall health – led him to believe that there was nothing wrong with me. He went further to posit a theory that I was punching myself in my sleep or sleeping on a closed hand that caused the trauma. Perhaps my wife was beating me after I passed out from drinking too much? He even offered a personal story from his boyhood as evidence of this possibility. I asked specifically if there was something inside my head that could cause the black eyes. I asked if I needed some kind of brain scan. He vehemently claimed that it was impossible for something in the head to cause bleeding on the face – the head was just not made this way. His assumptions and conclusions were all wrong.
If you do not like the answers you are getting, then examine the questions you are asking.
Still looking for answers I figured I needed a different kind of expert, one on the area around the eye and not one that just looked at the condition of the eye itself. I had no idea what kind of expert that would be and asked my kid’s optometrist. He recommended an ophthalmological surgeon who would have the expertise of the whole eye structure - the orbit – that contains the eyeball as well as optic nerves, etc. I stumbled across a brilliant doctor in Boca Raton by looking for the eye doctor office with the most number of doctors and ad space in the phone book. Most of these do cosmetic surgery, but they would have the right frame of reference I was looking for. Immediately in my first meeting with him he assumed there was something behind my eye and ordered an MRI that plainly showed the growing tumor there. I think he was brilliant because even though he could not immediately come up with a reason that an orbit tumor could cause the black eye, he went with what his analysis was telling him. He was surprisingly honest and open with me about this. He did later came up with a theory that the tumor was rubbing the walls of the orbit , rupturing small blood vessels that leaked blood into my face under the right eye causing the black eyes. Brilliant.
Even world-class experts have a hard time seeing beyond the focus of their expertise.
I was referred to the best orbit surgeon in the US to deal with the tumor. He treated me for what he assumed was a cavernous hemangioma (basically a knotting of blood vessels) in my right orbit. He planned surgery after waiting two months for the blood to clear up in the orbit. He never once brought up the idea that it was something else, a cancer tumor perhaps, even though his staff had my previous melanoma history. I believe the disconnect of giving my history to his staff and then only listening to his opinion in the few minutes allotted to me allowed this mistake to happen and is a potential downside of large teaching hospitals. I should have asked this question but I did not. I should have insisted on a biopsy and I should have sought a second opinion, but I did not. When I developed a skull lesion he continued with his treatment protocol. Even when, the Friday before my scheduled Tuesday eye surgery, a PET scan showed I had metastatic melanoma throughout my body, he still believed the evidence suggested it was a hemangioma and not a cancer metastasis. Was he covering his ass or just being stubborn? I learned from this the medical theory of unified diagnosis, which says you look for the diagnosis that explains as much of the problem as possible. The possibility that the eye tumor was a hemangioma while all my other tumors were metastasis was not unified. But he was an eye surgeon focused on removing the thing in my orbit and he was not looking for the reason why it was there. I made some mistakes here but thankfully it only cost me a couple months of diagnosis. Lesson learned.
Finding the right type of doctor does not mean you’ve found the right doctor.
My first oncologist was very unpleasant, but I know that an asshole doctor can also be a brilliant doctor so I stuck with him through my initial staging process. I found him after searching for the doctor at the regional cancer center that was most published, most involved in research and best known. He was indeed the expert on melanoma at that cancer center and I was fortunate to get an appointment with him, or so I thought. In his brusque manner he examined my PET scan and said I had to choose from one of four treatment options, with just a few sentences of explanation of each. He urged me to make a decision quickly, and even called a couple of times over the next week asking what my decision was. The options were all standard treatments with 0-15% response rates – chemo, high dose IL2, BRAF and Yervoy. He did not mention any of the other options out there, and although he was familiar with the t-cell therapy he said I was not a candidate because my tumors were not large enough to harvest. This was absolutely wrong, and the treatments he offered were standard and did not take anything into consideration about my specific health and condition. Indeed, he did not ask anything about my current health or general medical history. And when I told him I wanted an opinion from MD Anderson he said his cancer center could offer anything MD Anderson could. Wrong, wrong, wrong. I walked out of his office and never went back. Another doctor I know, when told about this, asked me what you call the person that graduated last in their class at medical school? “Doctor.”
Experts can be right and wrong at the same time.
My third opinion came from a well-known oncologist in Florida who was one of the nicest doctors I’ve met in my journey so far. He was very generous with his time and was very willing to argue the merits of different treatment protocols, but I believe he was wrong in his conclusions. Who am I to question a well-known oncology expert? Case in point, he said that biochemo treatment was proven academically as ineffective and that he had personal experience with the failure of the treatment to cure his patients. He asked me not to go through with it at MD Anderson. This really perplexed me and I dove into the scientific data for answers. I read many medical journals, often putting a “Dr.” in front of my name to get a trial subscription to the expensive ones. What did I find? After biochemo was first introduced and began making headlines it was rolled out across the country. A study of the resultant experience with biochemo found that the earlier stated results of 30%+ response rates were not being replicated and the toxic side effects were much more difficult to patients than earlier studies had stated. So the doctor was right? No. I also found a later study of this study’s results which showed that the treatment in the medical centers where there was biohemo expertise (Angeles, MD Anderson, etc. ) remained successful. The conclusion was that the expert staff at these centers – doctors and nurses with special training and experience with the protocol - could better help patients handle the side effects of the toxic treatment which allowed the patients to get higher doses that lead to higher results. Your local cancer treatment center could not achieve the higher doses as patients developed problems with the toxicity and therefore had the lower results. There is still controversy about this – I believe stemming from some kind of institutional inferiority complex of many regional cancer centers - but it made sense to me. It explained how he could be right and wrong and the same time. Additionally, I made an estimation of the demographics of this doctor’s practice which lead me to assume that most of his patients were elderly as it seemed to treat the large retirement population where it was located. He probably rarely had the healthy patient like me looking for rigorous treatment. His cancer treatment experience and expertise did not match my needs. He was right, but not right for me.
I’m not saying that I am not still making mistakes, but I always question assumptions – others and mine. The experience of cancer diagnosis is a scary one, more so than the actual treatment protocols. I've heard it described as being transported to another country. One day you are making coffee before work, taking your kids to school and planning your weekend. The next day after diagnosis you are alone in a foreign land where everybody speaks a different language. There are many people willing to help you, offering to show you the way home. But the path home is painted in the art of self reliance. That is the current state of cancer care, like it or not.
Cancer is not going to get an easy break from a misinformed doctor. Not with me. Not now. Not ever.
Monday, July 11, 2011
The Big Guns and the God of Thunder
OK, so it is time to bring out the big guns for this fight with cancer. I mentioned the TIL clinical trial before and I've gotten a lot of questions about it. On the right side and down a bit are permanent links to the study details and a great article about the process and Dr. Steven Rosenberg at the National Cancer Institute that developed it. Dr. Hwu at MD Anderson used to be at NCI and brought the study with him to Texas. The article in particular does the research work more justice than I can do here, but I'll give it a college try. The TIL study utilizes adoptive cell therapy (ACT) which is also call T-cell therapy. The acronym TIL stands for tumor infiltrating lymphocytes, my personal favorite because it sounds like a covert special operations military unit led by Steven Seagal. My understanding is that in every melanoma tumor lesion there are some immune cells trying to do the job. They are in the tumor but obviously they are not doing a good enough job because the tumor is growing, and that if we could reinforce these t-cells the body can successfully beat back the cancer. The process developed at NCI involves removing some tumors and extracting these t-cells from within them and then growing the t-cells in vitro in a lab. Then, to prepare the body for the new t-cells, they wipe out the body's entire immune system (lympho depletion) and replace it with the new t-cells. The result is a cancer patient with a new immune system specifically trained to fight melanoma, and that immune system will fight that cancer for the rest of its life. The durable results are over 50%, which is amazing compared to the other standard treatments that have a 5-15% response rate. Many researchers believe this is the future of fighting cancer, even a potential cure, but up to now very few people have undergone the treatment (about 95 at NCI, 45 at MD Anderson and some others at a research center in Israel). The reason so few have undergone the treatment, and that the clinical trial has not moved on from Stage 2, is that the patient needs to have an accessible tumor, t-cells that will grow in the lab and be strong enough to handle the tough treatment. The list of health factors required to be considered for the study is 23 items long with 8 exclusionary criteria. These criteria eliminate four of five potential candidates. Fortunately for me, I meet all of those. The treatment is also terribly expensive and is currently being undertaken at only the three research centers mentioned.
My treatment at MD Anderson will start with seven days of lympho depletion with chemo therapy (fludarabine and cytoxan). I'll be in sort of an isolation setting, we don't want anyone sneezing on me at this stage. The lympho depletion is is supposed to be easier than the biochemo protocol I already underwent and Dr. Patel is even working on getting a stationary bike into my treatment room for that phase (her estimation of my constitution is refreshing). Then, they'll grow the t-cells from the existing frozen millions into the billions in a special laboratory in Houston. On Day 0 they reintroduce the cells into my body. Then up to a week of consecutive high-dose interleukin (IL2) treatments, a biologic drug that will kick-start my new immune system into high gear and help my body to start utilizing the t-cells. This has similar side effects as biochemo and is no picnic. Low dose IL2 was a not to pleasant part of the cocktail in the biochemo I've already gone through so I'm sure high dose IL2 is even more fun. They want to give me as many high dose IL2 treatments as I can stand (specifically what my liver and heart can stand) up to 15 doses, most patients get 5-10 doses. I told the docs to give me 15 even if I am unconscious to which they smiled as if to a child asking to go to the moon, but I think a little bravado - however unwarranted - goes a long way in reinforcing my commitment to this treatment. I'll spend a few days to a week recovering in the hospital and then I'll go home for a couple weeks. Then I go back to Texas and we do the high dose IL2 treatment a second time. And then we wait, because the new immune system will take time to seek out and destroy the cancer. The next scans will be in six and twelve weeks after the "birth" of my new immune system where we’ll see if there is any progress. It may take many months before we start seeing results. It is interesting that my new immune system will be the same as a newborn's and I'll lose all my existing immunities that I've worked so hard to develop. That means next year I'll need measles, mumps and chicken pox inoculations. It will be interesting to be sitting in the pediatric office waiting room next year with a bunch of toddlers.
I believe cycling, and very often professional bike racing, to be an accurate metaphor for so many things that happen in life. In Stage 3 of this year's Tour de France Tyler Farrar, the best sprinter America has ever produced, looked like a possible to win the stage. It was also July 4th and for an American on an American team to win the stage that day would be a phenomenal achievement. However, the odds were long and Tyler faced many stronger and faster foes also fighting for the stage. The racing had been touchy and a tour-ending, or even career-ending, crash was a definite possibility. On Tyler's team is Thor Hushvold, the Norwegian "god of thunder" who was wearing the yellow jersey as the overall race leader in the Tour de France. Thor also wears the rainbow jersey signifying that he is the current reigning world champion road racer. Coming in together to the hectic last half kilometer of the stage, Thor jumped through a blind corner towing Tyler to the front of the nervous pack. I've never seen a yellow jersey lead out a sprinter at a Tour de France but Thor is like that, a team player confident of his world-best skills and always willing to jump after any potential victory. After Thor gave it his all he pulled over and let Tyler go on to sprint the final meters against his foes to win the biggest stage victory of his life. You can see Thor smiling in this picture, resplendent in his yellow jersey, a few riders back from Tyler. In many ways MD Anderson, and Dr. Patel, is my yellow jersey teammate leading me into the final section of the most important race of my life. They are world champions in fighting cancer and they go aggressively after any possibility of victory. And I know that they can get me close - closer than anyone else - but it is critical to remember that victory will require me to sprint the final meters alone and I know this will take everything I have. But I also know that cancer will not beat me to the line, cannot beat me to the line, when I have a world champion leading me into the finish.
My treatment at MD Anderson will start with seven days of lympho depletion with chemo therapy (fludarabine and cytoxan). I'll be in sort of an isolation setting, we don't want anyone sneezing on me at this stage. The lympho depletion is is supposed to be easier than the biochemo protocol I already underwent and Dr. Patel is even working on getting a stationary bike into my treatment room for that phase (her estimation of my constitution is refreshing). Then, they'll grow the t-cells from the existing frozen millions into the billions in a special laboratory in Houston. On Day 0 they reintroduce the cells into my body. Then up to a week of consecutive high-dose interleukin (IL2) treatments, a biologic drug that will kick-start my new immune system into high gear and help my body to start utilizing the t-cells. This has similar side effects as biochemo and is no picnic. Low dose IL2 was a not to pleasant part of the cocktail in the biochemo I've already gone through so I'm sure high dose IL2 is even more fun. They want to give me as many high dose IL2 treatments as I can stand (specifically what my liver and heart can stand) up to 15 doses, most patients get 5-10 doses. I told the docs to give me 15 even if I am unconscious to which they smiled as if to a child asking to go to the moon, but I think a little bravado - however unwarranted - goes a long way in reinforcing my commitment to this treatment. I'll spend a few days to a week recovering in the hospital and then I'll go home for a couple weeks. Then I go back to Texas and we do the high dose IL2 treatment a second time. And then we wait, because the new immune system will take time to seek out and destroy the cancer. The next scans will be in six and twelve weeks after the "birth" of my new immune system where we’ll see if there is any progress. It may take many months before we start seeing results. It is interesting that my new immune system will be the same as a newborn's and I'll lose all my existing immunities that I've worked so hard to develop. That means next year I'll need measles, mumps and chicken pox inoculations. It will be interesting to be sitting in the pediatric office waiting room next year with a bunch of toddlers.
I believe cycling, and very often professional bike racing, to be an accurate metaphor for so many things that happen in life. In Stage 3 of this year's Tour de France Tyler Farrar, the best sprinter America has ever produced, looked like a possible to win the stage. It was also July 4th and for an American on an American team to win the stage that day would be a phenomenal achievement. However, the odds were long and Tyler faced many stronger and faster foes also fighting for the stage. The racing had been touchy and a tour-ending, or even career-ending, crash was a definite possibility. On Tyler's team is Thor Hushvold, the Norwegian "god of thunder" who was wearing the yellow jersey as the overall race leader in the Tour de France. Thor also wears the rainbow jersey signifying that he is the current reigning world champion road racer. Coming in together to the hectic last half kilometer of the stage, Thor jumped through a blind corner towing Tyler to the front of the nervous pack. I've never seen a yellow jersey lead out a sprinter at a Tour de France but Thor is like that, a team player confident of his world-best skills and always willing to jump after any potential victory. After Thor gave it his all he pulled over and let Tyler go on to sprint the final meters against his foes to win the biggest stage victory of his life. You can see Thor smiling in this picture, resplendent in his yellow jersey, a few riders back from Tyler. In many ways MD Anderson, and Dr. Patel, is my yellow jersey teammate leading me into the final section of the most important race of my life. They are world champions in fighting cancer and they go aggressively after any possibility of victory. And I know that they can get me close - closer than anyone else - but it is critical to remember that victory will require me to sprint the final meters alone and I know this will take everything I have. But I also know that cancer will not beat me to the line, cannot beat me to the line, when I have a world champion leading me into the finish.
Saturday, July 2, 2011
Scan Results
Well, we got the results yesterday of Thursdays CT and MRIs and we got neither a winning lottery ticket nor devastating news - something more in the middle and along the lines of our original treatment plan. The biochemo did not shrink my existing tumors but they also did not grow. The tumor in my hip looks stable enough that Dr. Patel approved a stationary bike for me, which is pretty exciting. Unfortunately, we did find two new tumors near my kidney. Sometimes they call biochemo a "springboard treatment" specifically because it halts the progress of your existing cancer while you have to wait for other treatment options. For us, we've waited five weeks for our other treatment option – the TIL study - and the t-cells they extracted from me in May have grown successfully into the millions. This means that I can likely enter the TIL clinical trial at the end of July. More details on what's involved in that later.
So, what does this news mean? Its some cold comfort that this was the plan from day one. The TIL study was my number one goal and the reason we went to MD Anderson, but we did not get the sudden success from the biochemo that we held as an outside hope. Our recent optimism was born of my surprisingly strong recovery from the biochemo. We were made to expect to limp through the time in between treatments, to expect blood transfusions and emergency room visits, but my recovery was rapid and complete. Now, two weeks after my second round - which was supposed to be the worst - I feel the best I have since entering treatment. I even hit the hotel gym before seeing Dr. Patel yesterday. I do not think my stamina was working in the same direction as the biochemo treatment. Chemo works by destroying you - hoping that the healthy part of you is destroyed a little less than the cancer part of you. The TIL treatment, however, relies on your body’s ability to fight, to recover and to attack that which attacks it. This treatment seems to play into my strengths.
Switching to the TIL treatment has many other positives. In addition to having a complete attack plan, it means that I'll be spending a wonderful bonus time at home with the family while I'm feeling good. It also means I may return to work after recovering from the second IL2 treatment and that I can resume a relatively normal life until otherwise notified. This is all good news but delivered with a bit of a setback. Lance said that cancer taught him to be comfortable with ambiguity, now I know what he's talking about.
So this week we're going to take the kids to Disney World and enjoy the downtime before the big attack in a couple of weeks. I'll continue regaining my stamina and getting stronger and healthier each and every day. Meanwhile, cancer can sit there and wait, nervously anticipating the billions of specially trained tumor infiltrating lymphocytes that are coming its way soon. Think about how many zeros are in a billion, cancer, and I'll be enjoying the Magic Kingdom.
Tuesday, June 28, 2011
Pre test results, pre the Grande Boucle
Ann and I are heading off to Houston, Texas, tomorrow for CT and MRI scans on Thursday. The scans will show if there has been any progress made in fighting the cancer, or if cancer has made any progress on me by growing and infiltrating more of my body. The main focus will be on the tumor in my lung, which is kind of floating there and easy to measure and compare from the March PET scans. On Friday, my case will be reviewed and we’ll meet with Dr. Patel to review the results and make a battle plan. If biochemo therapy is working then we’ll continue with a third round of biochemo starting next Friday. If it is not working, we’ll likely switch it up and I’ll enter the TIL (tumor infiltrating lymphocyte) clinical trial at MD Anderson next Friday. Not sure what we’ll do if there is no result at all. I recently read a blog called Melanoma Mom of a young woman with a very similar case to mine where her two treatments prior to entering the TIL study actually shrunk her tumors enough to avert the need for anything else, so there’s as much chance of great news as of bad. Needless to say we are on pins and needles awaiting the results. All I can say is that I feel great now, two weeks after my last biochemo treatment, and I know my body has been busy kicking cancer’s ass. I’ll let you know the results over the weekend.
Also this weekend is, much to my wife’s dismay, the start of the 98th Tour de France. Being a cyclist and pro cycling fan this means 23 days of the most amazing performances of individuals and teams, epic battles steeped in a hundred years of tradition across 2,131 miles of the beautiful fields and mountains of France. And very dear to my heart is the greatest cyclist in the history of le Tour, seven-time winner Lance Armstrong. Especially so this week, pre-results, as I consider what my cancer diagnosis means to me. I believe in the bottom of my heart that we ultimately determine what things mean to us and that in turn determines our future. Life’s roadblocks, setbacks and failures have more of an impact on our lives than successes and bouts of contentment. This setback in my health has the potential to have an enormous effect on my life, and that can be a negative or positive. I’ve determined, and am committed, that it will be positive. I will come out the other end of this fight a better man, a stronger father and more loving husband. I'll come out a more complete human being with a new fire burning in my gut to try to prevent this from happening to others. In short, this will be a turning point for me, a lesson in life that I’ll take to heart to make my life – and hopefully that of others – better and more complete. And I’m not alone, studies show that most cancer survivors come away from cancer with a sense of blessing. Lance Armstrong was crystal clear on what cancer meant to him. He said:
“Without cancer I would have never won a single Tour de France. Cancer taught me a plan for purposeful living, even that in turn taught me how to train and win purposefully. It taught me that pain has a reason, and that sometimes the experience of losing things – whether health or a car or an old sense of self – has its own value in the scheme of life. Pain and loss are great enhancers.”
Whatever the results on Friday, I know – beyond a shadow of a doubt – that having cancer is going to make me a better person. Take that cancer, and stick it where the sun don’t shine.
Thursday, June 23, 2011
Downtime
In a war, troops are not always engaged in combat, but they are always fighting. Time spent behind the lines is a weird kind of limbo, knowing that a life and death battle rages on just over the horizon but spending a lot of time just hanging out. I guess many of you are wondering what I do with myself in between treatments. Well, spending time at home has been an interesting exercise in both trying to get stuff done as well as filling up the time of the day. This is made all the more complicated by a combination of lack of ability to do things you could, and wanted, to do before and all the time off from work to get treatment. I used to budget out every minute of my time, planning out my schedule three months in advance in thirty minute increments with color coded graphics and synchronized calendar files. Now, for the first time since I was in college, I find each day between treatments a relatively blank slate. I'm not going to work, not riding my bike, not going out and that frees up about 99.6% of my non-family time. If you think that what you do does not define who you are then you should try taking some serious time off from all that you do, it’s an eye opener. Now I'm not a finance executive, not a cyclist, not a not a stranger to a glass in my hand (at least for now). I wonder if I met someone new how I would describe myself? To help answer that question I’ve been spending some serious time developing an attitude of gratitude, and defining who I am by all that I am blessed with instead of all that I do. For all I've lost so far I am still a seriously lucky dude. Two healthy, perfect girls and a wonderful wife would make it all worthwhile but I have so much more - including the relative good health to fight this cancer. To whit, I've started a morning routine of walking the dogs one mile followed by yoga and core exercise (balance board, etc.). I started setting my alarm clock and taking showers on a regular basis and trying to maintain some discipline while in the rear with the gear. Chemo brain still makes anything intellectual a challenge, but I can fight cancer every day between treatments with push-ups and sit-ups. I am still watching massive amounts of the Military Channel and Versus Cycling TV as well as afternoon napping with the dogs, but working on speeding my recovery is going to help me beat this thing. So in between treatments I'm spending my time continuing the fight. I'm rebuilding reserves, continuing to research treatment options and tactics, licking my wounds and readying for the next attack.
Sunday, June 19, 2011
Dad Day
Well, round 2 done. OK, I may not have been doing pushups in the corner but I made it through the entire decrescendo course of biochemo without missing any of the drugs (last time they pulled me short of the last vinplastin and Interferon doses because of low blood counts). I insisted on every drop this time. It was rough but I think I came out of it in better shape than last round. I’m weak, my skin is peeling like an Ohio tourist on their first spring break to Panama City, but I’m overall in good shape. I had my PICC line removed, so no cyborg plugs. I have two weeks at home to enjoy being a husband and father. Thanks for all the good wishes during my hospital stay; I wish I could respond to all of you but for some I don’t have e-mails. But remember that each and every message means so very much to me.
So, the good news. My t-cells grew in sufficient quantities to enter the TIL study (detailed below, link on the right), yeah! They have been frozen and await further instructions. On June 30th Ann and I return to MD Anderson for imaging, CT scans of the whole body, to see if we’ve made any progress against the cancer or if cancer has made any progress against me. If the biochemo shows progress we may stick to it, starting a third round on July 8th. If no progress, or negative progress, than we’ll likely plan to enter the TIL study at about the same time. Either way, cancer gets some more ass kicking but this could be the beginning of the end or just the end of the beginning. July 1st will tell, and boy is that going to be an ominous meeting with Dr. Patel.
Today is Father’s Day and the topic has been weighing on me the past weeks. As I lay in the hospital the duties of fatherhood went on untended except by my overburdened wife. The pool pump broke, the insurance check was not right, the kids toy castle needed rebuilding. Cancer has taken away much of my functionality of what the role of father and provider means to me, at least temporarily. Any guy will tell you how this cuts deep, how the inadequacy weighs down on you like a ton of soft bricks. Husband is bad but falling down on father duties seems all the more difficult to swallow. All I can do is contribute where I can, support those supporting me, and vow to come back as a better father and provider when this battle is finally drawn to a close. I relish this bit of shame, and use it as fuel for the fight when I ever lack some spark. But today, on father’s day, when I see the unbridled joy in Gwen and Sabrina’s eyes when they play with me, I remember that what I may temporarily lack in being a father is not the entirety of the role. Any man can be a Father but it takes someone special to be a Dad, and cancer cannot take that away from me.
Subscribe to:
Comments (Atom)